By Christina Marvin
Immunotherapy is an entirely new way of thinking about cancer treatment. Traditional therapies such as surgery, chemotherapy, and radiation aim to target and destroy tumors. Often times, tumor targeting is poor or the treatments damage other parts of the body. Immunotherapy, on the other hand, teaches our body’s natural defenses (the immune system) to recognize and eliminate tumors.
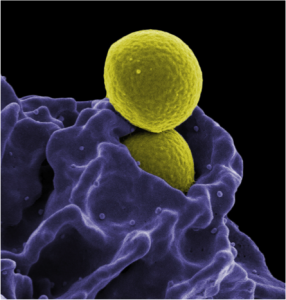
A macrophage, part of the human immune system, eliminating bacteria from the body. For decades, cancer treatment has relied on surgery, radiation, and chemotherapy. However, immunotherapy may allow our body’s immune defense to attack and eliminate cancer cells like it attacks foreign invaders.
Cancer treatment has never been easy. In his 1971 State of the Union address, President Richard Nixon officially launched the war on cancer by encouraging the use of federal funds for basic research and treatment. Since then, over $90 billion in federal money has been spent on the study of cancer. Despite continued efforts in therapy development, doctors have treated cancer the same way for decades, often resulting in serious side effects. Traditional surgery and radiation are associated with debilitating side effects. Chemotherapeutics, while effective initially, can cause serious illnesses and eventually become ineffective at killing the cancer.
However, over the past three years, interest has grown in a new treatment that some scientists claim will be the next major breakthrough in the war on cancer: immunotherapy.
Our immune system is a collection of cells, tissues, and organs that ward off foreign germs and infections in order to keep us healthy. In other words, it is like the police force of our body. Although tumor cells are our own cells, they have been severely mutated. Under normal conditions, the immune system should recognize the mutated cells as unnatural and eliminate them as if they were foreign material.
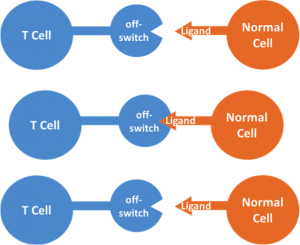
T cells patrol the body, searching for foreign or unnatural invaders. When a T cell encounters another cell, it looks for a certain ligand that signifies the other cell is normal. If the off switch finds the ligand, the T cells mark the other cell as normal and move on. Often times, tumor cells cloak themselves in ligands that trick the T cells into thinking they are normal.
If our immune system is such a good watch dog, why does it allow tumors to grow in the first place? The answer lies in the ability of tumor cells to disguise themselves as normal cells. T cells are a major driving force in the immune system because they contain receptors that recognize foreign invaders. They also contain “off switches”, or checkpoints, that prevent them from attacking normal cells. These off switches are receptors that recognize a certain ligand partner on another cell. If the off switch sees the ligand on the other cell, the T cell marks it as normal and leaves it alone. Tumor cells like to cloak themselves in ligands and trick the immune system into thinking the tumor cells are normal cells. The most common type of immunotherapy relies on uncloaking the tumor to make it visible to the immune system.
Checkpoint inhibitors block the interaction that tricks the T cells by getting in the way. Imagine that the off switch and its ligand are puzzle pieces that fit together. Although the inhibitor does nothing biologically, it looks exactly like a puzzle piece. The inhibitor fits perfectly into the puzzle, but the puzzle cannot really be completed since the real piece is now blocked. Checkpoint inhibitor therapy uses inhibitors to block either the off switch on the T cell, or the ligand on the tumor cells. Because T cells no longer receive the signal that they are dealing with normal cells, the tumor’s disguise is revealed and the immune system proceeds to destroy the cancer.
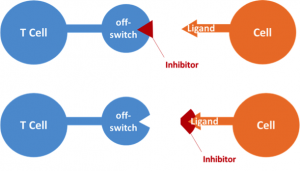
Checkpoint inhibitors block the interaction between the T cell’s off switch and the tumor cell’s ligand. Since the T cell cannot mark the tumor cell as normal, it calls in other parts of the immune system to attack the unnatural cell.
In some individuals, the clinical results of checkpoint inhibitors have been outstanding, sending tumors into remission and extending life expectancy by years. However, the therapy has only been a miracle for some. Scientists continue to investigate why immunotherapy works so well for a few people, while failing for the majority. This inconsistency is a major obstacle for doctors who want to broaden the use of immunotherapy. Personalized medicine classifies patients based on genetics and uses that information to predict a patient’s response to specific treatments. This classification system may help the scientific community optimize immunotherapy and extend its therapeutic benefit to many more patients.
Edited by Michelle Engle and Tamara Vital
