By Jenna Beam
The microbiome is a complex network of microbes living in and on your body. This group of microbes is really important for helping you digest food, protecting your skin and gut from infections, and may even play a role in brain health. When people use the term microbiome, they are often describing the billions of bacteria living on and in your body. But did you know that there are also fungi that naturally live in and on your body alongside the bacteria?
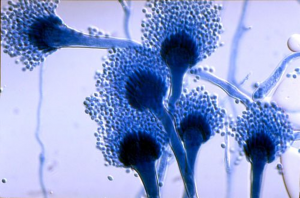
When I learned about fungi in school, I learned about them as decomposers – you know, the slimy mushrooms growing on dead trees. And while ALL mushrooms are fungi, not all fungi are mushrooms. Some notable fungi that don’t form mushrooms you might have heard of are black mold (see Image 1) and the fungus that produces the antibiotic penicillin (a little history on that can be found here)! Some fungi help plants get nutrients, while other fungi can cause a wide range of diseases, like Cryphonectria parasitica (read about it here).
There are also fungi on and in us that make up our typical microbiome (sometimes called the “mycobiome”) and others that can cause diseases. One example of a disease-causing fungus is Aspergillus fumigatus, which causes the disease aspergillosis. While anyone can get a fungal infection, people with weakened immune systems are especially at risk for A. fumigatus. This includes cancer patients, patients with the genetic disorder cystic fibrosis, as well as people getting organ transplants.
A. fumigatus is very common in soil and compost piles and is really important for parts of the carbon and nitrogen cycles. When the fungus is growing, it forms conidiophores, or bunches of tiny particles called “conidia” on the end of a stalk or filament (see Image 2). The conidia are pretty similar to spores and are easily released into the air where they can be inhaled. Most of the time, your innate immune system does exactly what it’s supposed to do and simply destroys the conidia before they can cause an infection. Sometimes, however, like in the case of aspergillosis, the immune system isn’t able to destroy the conidia. Instead, the conidia “wake up” and start growing into long, thin structures called hyphae (pronounced high-fee). The hyphae can start to grow through the lung tissue and into blood vessels. Pretty gross. This can lead to swelling and inflammation, causing coughing, wheezing and chest pain.
Just like we can treat bacterial infections with antibiotics, fungal infections can be treated with antifungals. However, antifungals don’t always work and treatment for aspergillosis may also include steroids and surgery, depending on how severe the disease is. Because some patients have to be on antifungals for a long time, antifungal resistance in A. fumigatus is becoming a big problem. Lucky for us, scientists are working hard to improve antifungal treatment, as well as finding alternatives to antifungals. Maybe one day we’ll even be able to prevent these infections from happening in the first place!
Edited by Anna Wheless and Carolina Herrera